mRNA Vaccines Moonshot
mRNA vaccines changed the course of the COVID-19 pandemic. Now GW researchers are developing these vaccines to treat and prevent diseases from cancer and HIV to malaria and shingles.
Story // Sarah C.P. Williams
Long before a mysterious, pneumonia-like illness grew into a global pandemic—and long before an array of vaccines emerged to halt COVID-19 in its tracks—scientists were experimenting with messenger RNA (mRNA) vaccines.
Unlike some classical vaccines that introduce a dead or weakened part of a pathogen into the body to generate a protective immune response, mRNA vaccines instruct the body’s own cells to make a protein that the body recognizes as unfamiliar, and the immune system goes into action. With classical vaccines and mRNA vaccines, the end goal is the same—to train the body’s immune system to detect and dispense with a pathogen—but many scientists working on mRNA vaccines believe they might be easier and less expensive to manufacture as well as more effective.
The first mRNA vaccines against influenza were tested in mice in the 1990s, and by the early 2000s, cancer researchers were developing mRNA vaccines to target tumors. Once scientists figured out how to enclose the fragile mRNA molecule inside a lipid nanoparticle—a fatty sphere that acts as a tiny delivery vehicle—to keep it from degrading in the body before delivering its instructions to cells, research began to pick up even more. Still, for decades, vaccine research and development remained slow and expensive.
Then the COVID-19 pandemic hit. Scientists and pharmaceutical companies that had been working on mRNA vaccines for years saw how their technology’s speed and versatility could help fight the new coronavirus. Just 42 days after the publication of the genetic sequence of the SARS-CoV-2 virus, the pharmaceutical company Moderna Therapeutics shipped its first mRNA vaccine against COVID-19 to the National Institutes of Health to administer to volunteers. Later in 2020, GW was selected as one of the clinical vaccine sites to test that same vaccine in a Phase 3 trial, the final step before a vaccine can be submitted to a regulatory body for approval.
“As soon as I saw how quickly we were able to develop and study the COVID-19 vaccines, I knew this technology was absolutely going to be a boon for the broader field of vaccine development,” says David Diemert, professor of medicine at the GW School of Medicine and Health Sciences and clinical director of the GW Vaccine Research Unit.
That prediction was right. The efficacy of mRNA vaccines against COVID-19 on a global level has ushered in a new era of innovation. Researchers can design and test vaccines against nearly any pathogen in a matter of weeks, using a versatile mRNA platform that is considered incredibly safe.
At GW, the mRNA vaccines being developed and tested in clinical trials have lofty goals—eradicating malaria, treating aggressive cancer and preventing HIV, among them.
A New Way to Deliver a “Trojan Horse”
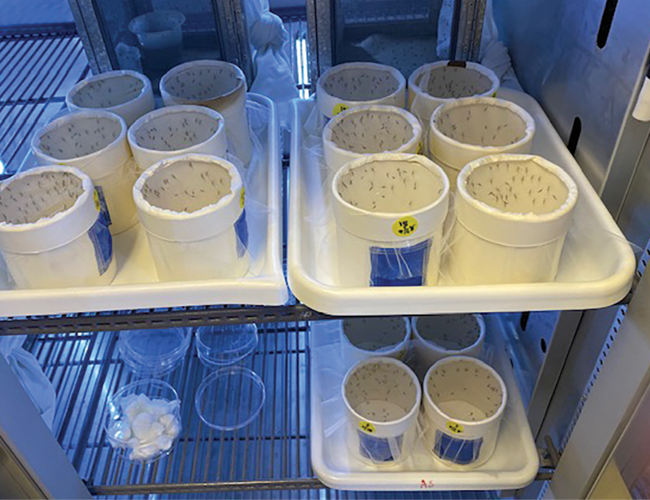
In Nirbhay Kumar’s native India, the monsoons come every summer. And with the monsoons—mosquitoes and malaria. As they suck blood, infected female mosquitoes inject the malaria parasite into humans. Hundreds of millions of people around the world are infected with malaria each year, and more than half a million people die of the disease, mostly in sub-Saharan Africa but also dozens of other countries.
Kumar, a professor of global health at the GW Milken Institute School of Public Health, was drawn to studying malaria because of its public health impact in India. Now he’s spent 40 years working to fight the parasite.
“During that time, there has been a lot of progress, and we have seen dozens of countries eliminate malaria,” he says. “But we also see the malaria parasites continuously evolving to become drug resistant. Sooner or later, we once again may not have any effective drugs to treat malaria.”
In 2021, the World Health Organization endorsed the first malaria vaccine. According to Kumar, however, the vaccine is not as effective as most would like—it prevents disease in about a third of the people who receive it and wears off in a matter of months. “We definitely don’t have an ideal vaccine yet,” he says.
“Even today, I’m astonished at how effective these vaccines are. They’re at least 10 times more effective than the DNA vaccines I was working on.”
- Nirbhay Kumar
Professor, Global Health
The vaccines Kumar has developed over the years take multiple approaches to blocking malaria. Some trigger antibodies that stop malaria from reproducing in a person’s liver and causing infection. But others lead to antibodies that block the malaria parasite from maturing in mosquito guts. Alone, this kind of vaccine isn’t designed to prevent disease in a person who receives it but instead works to stop malaria at a broader scale. When a mosquito bites a vaccinated person, they receive something akin to a Trojan horse: blood containing not only malaria parasites but also antibodies that stop the parasite from getting any further in its life cycle.
“The idea is to basically stop the malaria transmission cycle so that we can reduce the number of infected mosquitoes,” says Kumar. “Fewer infected mosquitoes, over time, means fewer infected people.”
In the 1980s and 1990s, however, Kumar struggled to make these vaccines a reality because of the challenges of producing protein-based vaccines—the same struggle that others in the vaccine development space were also facing. “Some of these malaria proteins are incredibly difficult to manufacture,” he says.
Over the following years, researchers, including Kumar, began to experiment with DNA-based vaccines that delivered genetic material, rather than proteins, to human cells. The cells themselves could produce the corresponding protein to trigger an immune response. But to work, DNA vaccines must sneak into the tightly guarded central nuclei of cells where DNA is stored—a difficult task requiring small pulses of electricity to be administered with the strands of DNA. Kumar wasn’t sure patients would ever agree to this kind of shot.
Then, at a vaccine conference in 2019, Kumar saw a presentation by Drew Weissman of the University of Pennsylvania on mRNA-based vaccines for influenza. He was immediately intrigued.
Information in cells flows from DNA to mRNA to protein. mRNA is copied from a cell’s master DNA and then leaves the nuclei of cells to be translated into proteins. That means an mRNA vaccine has the same information as DNA but, to yield proteins, needs only get into cells, not their difficult-to-access cell nuclei.
“If you use mRNA, you completely bypass this delivery process we’d been struggling with,” Kumar says. “I sought out Drew after his talk, and the first thing I asked him was whether we could do this for malaria.”
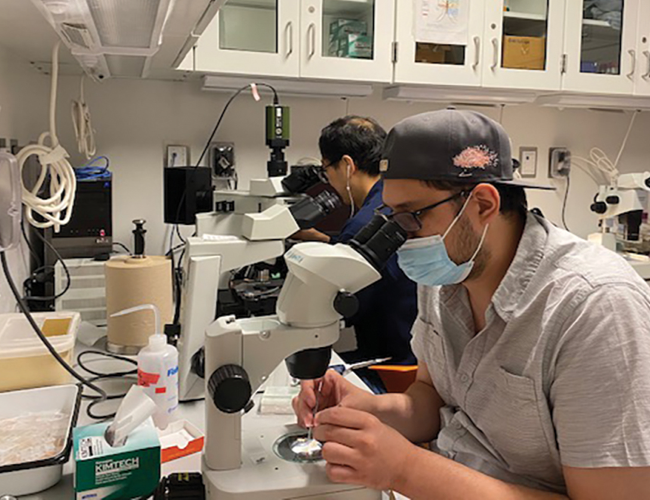
Kumar's research team in the insectary lab on campus. Kumar has spent four decades working to combat malaria, a public health menace in his native India.
Kumar and Weissman began collaborating and, after a break for COVID-19, produced experimental mRNA vaccines against two malaria proteins that Kumar had long studied—one that blocks human infection and a second that blocks the malaria parasite’s development in mosquitoes. Both proteins are from Plasmodium falciparum, one of the four parasite species that cause malaria.
Last year, the researchers reported in the journal npj Vaccines that their combination mRNA vaccine was incredibly effective at preventing P. falciparum infections in animals and nearly 100% effective in blocking mosquito-to-mosquito transmission.
“Even today, I’m astonished at how effective these vaccines are,” says Kumar. “They’re at least 10 times more effective than the DNA vaccines I was working on, and they take a fraction of the time to manufacture compared to classic protein-based vaccines.”
Weissman, who also works on vaccine development for many other health conditions, says that the malaria vaccine is a perfect example of the promise of mRNA vaccines.
“Malaria is a major concern that previous vaccines have poorly addressed. The ease of producing this vaccine and its effectiveness were both very exciting,” he says. “The mRNA platform has enormous potential to treat many diseases, including vaccines for infectious diseases, autoimmunity, allergies and cancer.”
A Personal, Precise Approach
In 2019, Julie Bauman, now a professor of medicine at the GW School of Medicine and Health Sciences and director of the GW Cancer Center, enrolled a new patient in a clinical trial to test a personalized cancer vaccine made by pharmaceutical company Moderna, in combination with an FDA-approved immunotherapy called pembrolizumab. The patient, a 35-year-old mother in Arizona with an aggressive form of head and neck cancer, was planning her own funeral. Standard chemotherapy and surgery had failed to contain the cancer, which had now spread to her lungs. As a last resort, she signed up for the trial.
While many vaccines are designed to prevent disease—you receive shots so that you never get sick with measles or tetanus, for instance—cancer vaccines instead aim to treat existing disease by teaching the immune system to recognize cancer-related proteins as foreign invaders.
“I think the idea of harnessing our own natural immunity appeals to everyone because cancer feels like such a betrayal,” says Bauman, who came to GW in 2022 from the University of Arizona. “One of our own cells has betrayed us and threatened our very existence, but let’s waken our own immune system to eradicate it.”
“We’re at the beginning of a trajectory where we can target cancer in a much more precise and effective way.”
- Julie Bauman
Professor, Medicine
Director, GW Cancer Center
For the young mother enrolled in the clinical trial, the team compared a sample of her tumor with her healthy cells, pinpointing genes that had mutated and were different in the cancer. These mutations can act like flags to the immune system, signaling which cells are affected by cancer. In just a few weeks, a vaccine was designed to deliver these genes, in the form of mRNA, to the patient by an injection in the muscle. Because they don’t integrate into the genomes of human cells, the mRNA molecules themselves can’t cause cancer. Instead, immune cells take up the mRNA molecules, translate them into protein fragments, and educate the immune system that these protein “flags” should be destroyed. This spurs the immune system throughout the body to begin attacking the cancer cells containing the mutated proteins.
Twenty-seven weeks after she began receiving the mRNA vaccine, the patient’s cancer was gone. She was in complete remission.
Unlike the flurry of mRNA vaccines under development in the wake of COVID-19, these personalized cancer vaccines aren’t new—mRNA has been a mainstay in cancer vaccine research for nearly two decades.
“One of the reasons we were able to develop a COVID vaccine so quickly was actually because of the decades of research in cancer vaccination that preceded it,” says Bauman.
Bauman specializes in head and neck cancer, which has a high mortality rate when not diagnosed early. Ten of her patients, including the young mother from Arizona, were part of a Phase 1 trial run by the pharmaceutical company Moderna to test mRNA vaccines in combination with pembrolizumab. Five of the 10 patients saw their tumors shrink or disappear.
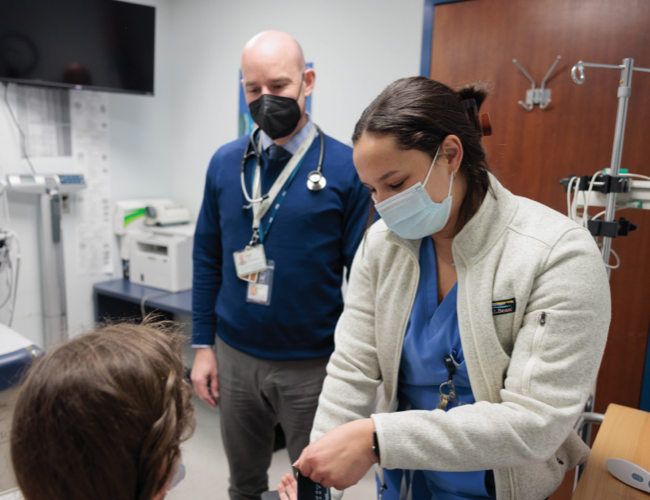
Julie Bauman aims to build better patient outcomes by bridging innovative, multidisciplinary research and clinical care. In 2022, Bauman was installed as the Dr. Cyrus Katzen Family Director of the GW Cancer Center (pictured right, with Jay Katzen).
At GW, Bauman will be opening the next phase of the clinical trial, evaluating the same personalized mRNA vaccine together with pembrolizumab in patients with advanced cases of several cancers, including pancreatic and head and neck cancer. The fact that each vaccine is individually matched to a patient’s own tumors makes it a novel and promising approach to fighting cancer, she says.
This summer, she and her colleagues at the GW Cancer Center also treated their first patient with a different kind of mRNA vaccine—one that encodes two immune proteins called IDO and PD-L1, which are often found at high levels in cancer cells and act like brakes on the immune system. The vaccine spurs the immune system to target IDO and PD-L1, enabling both direct immune killing of the cancer as well as wiping out the T cell brakes to increase other immune activity.
“I think in 20 years, we’ll look back and think that most of our cancer treatments before now were incredibly barbaric,” says Bauman. “But now, in part due to mRNA vaccines, we’re at the beginning of a trajectory where we can target cancer in a much more precise and effective way.”
Infectious disease doctor David Diemert, professor of medicine at the GW School of Medicine and Health Sciences and clinical director of the GW Vaccine Research Unit (VRU), began his career studying malaria in West Africa and hookworm in rural Brazil. At the time, developing a vaccine mere months after the start of a pandemic or rapidly developing vaccines against neglected tropical diseases seemed almost impossible. mRNA vaccines are changing that.
Over the course of the last 20 years, Diemert and his colleagues at the GW VRU have built, from the ground up, the facilities and infrastructure to test the safety and efficacy of vaccines through clinical trials conducted at GW. In 2020, the VRU worked with the pharmaceutical companies Moderna and Sanofi to run Phase 2 and 3 trials of vaccines against the SARS-CoV-2 virus. It was the first time Diemert had worked with an mRNA vaccine, and he was astounded by how quickly the vaccine could be produced and how effective it ended up being.
“COVID-19 acted as proof of concept for mRNA vaccines in terms of both safety and how well they can elicit immune responses,” he says. “With mRNA vaccines, there’s absolutely no messing with someone’s DNA. The mRNA goes into cells, gets translated into protein and very quickly gets degraded.”
Before COVID-19, GW had been one of the first sites in the world to test a new generation of protein-based HIV vaccines, which coaxed people’s bodies into producing broadly neutralizing antibodies against part of HIV. (Broadly neutralizing means the antibodies recognize many strains of the virus, even as it quickly evolves.)
“COVID-19 acted as proof of concept for mRNA vaccines in terms of both safety and how well they can elicit immune responses.”
- David Diemert
Professor, Medicine
Clinical Director, GW Vaccine Research Unit
The Phase 1 trial was successful, showing that the vaccine was safe and triggered the production of a critical immune cell. But by the time the results of that study were published in 2022, Diemert and his colleagues at GW were already recruiting dozens of patients for the next version of the vaccine: an mRNA vaccine that is designed to make the body produce the same broadly neutralizing antibodies. Using an mRNA vaccine instead of a protein vaccine means the vaccine can be mass produced more easily and cheaply and—if it ever becomes ineffective against a strain of HIV—easily altered.
At the same time, Diemert is ramping up enrollment of patients in a Phase 1 trial of an mRNA-based shingles vaccine produced by Pfizer. The only shingles vaccine on the market today—a protein-based vaccine—has significant side effects for many recipients, and scientists think the mRNA version might lead to fewer side effects and be equally effective.
The quick pivots by pharmaceutical companies to develop these new mRNA vaccines in just a few years illustrate the speed and versatility of the technology, Diemert says. But it remains to be seen whether mRNA becomes the standard platform for all future vaccines or just one option in the menu of vaccine design components.
“There are still some open questions about the long-term effectiveness of mRNA vaccines and whether that’s any different than with protein-based vaccines,” he says. “As we move through all these other trials, I think those questions will get answered.”
David Diemert and other colleagues at GW led one of the clinical trials sites that played an essential role in developing a COVID-19 vaccine approved for emergency use during the pandemic.
Despite those questions, the promise of mRNA vaccines to halt the next pandemic, treat emerging pathogens and address epidemics around the world is real. Work on developing a new generation of experimental hookworm vaccines, for instance, is already underway at the VRU. The low cost and ease of production of the vaccines mean that they could be made on site in resource-limited countries.
“The World Health Organization and other international groups are laying the foundations for establishing mRNA vaccine research and manufacturing facilities in places like sub-Saharan Africa to nimbly respond to future emerging infections such as the Marburg and Ebola hemorrhagic fever viruses,” says Diemert.
For researchers such as Diemert, Bauman and Kumar, mRNA vaccines represent a highly promising and potent new defense against some of the world’s most enduring and lethal diseases.
Curing cancer and HIV or eradicating malaria may have once seemed like moonshot-level aspirations, but they could be on the verge of becoming achievable realities with an assist from mRNA vaccines.
Photography:
Battling Malaria: Nirbhay Kumar
Combatting Cancer: Rich Riggins/William Atkins
Pursuing Immunity: Harrison Jones/William Atkins